The Hidden Crisis in Mouth Cancer: Why Prevention Is the New Cure
Why is one of the world’s deadliest cancers still missing from prevention efforts?
The following article is an opinion piece written by Sam Whitehouse, PhD. The views and opinions expressed in this article are those of the author and do not necessarily reflect the official position of Technology Networks.
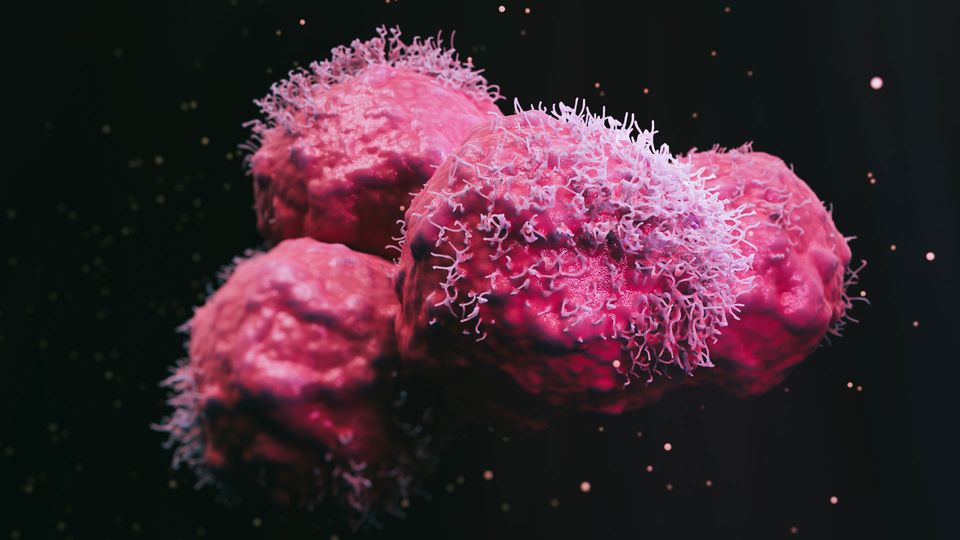
Oral cancer – commonly known as mouth cancer – is the sixth most common cancer worldwide and has a five-year survival rate lower than many other cancers. The main reason for this poor prognosis is that the disease is often detected much too late, and there are very few treatment options available once it is diagnosed. So why does a cancer with one of the worst survival rates remain largely underrepresented both in public health discourse and innovation pipelines?
While oncology on the whole is increasingly shifting towards early detection and prevention models, oral cancer remains stuck in a reactive, late-stage care model. It’s time we apply the same urgency and innovation to this overlooked disease, particularly in terms of scalable, early interventions.
Mouth cancer: The blind spot in oncology
Globally, the incidence of mouth cancer is rising, causing approximately 180,000 deaths each year. The disease disproportionately affects lower socioeconomic groups, particularly populations in low- and middle-income countries (LMICs), where tobacco and alcohol use is high but access to healthcare is low. In India, for example, it is the leading cause of cancer-related deaths among men.
But this is not just a problem confined to LMICs. Mouth cancer is also prevalent in countries such as the UK, Australia and North America. In places like Hong Kong, the misconception that “we don’t really get that here” persists – despite evidence to the contrary. A major part of the problem is that oral cancer lacks the visibility of other cancers, meaning it receives less funding and public attention.
This disease is aggressive and often fatal. Survival rates drop dramatically beyond five years after diagnosis, and many who survive face long-term effects such as facial disfigurement or speech loss. These consequences make it harder for survivors to share their experiences, contributing to a lack of public awareness.
Crucially, many of these deaths are preventable. Early detection and intervention can significantly improve outcomes, yet structured screening programs remain rare – especially in regions with the highest burden. Even in high-income countries, oral cancer is frequently excluded from national cancer strategies, early diagnosis initiatives and public health campaigns.
The result is a growing equity gap, where most resources are channeled into treating advanced disease rather than preventing it in the first place – creating a high economic and human cost. Prioritizing simple, scalable screening approaches – especially in high-risk communities – could save lives and reduce suffering.
Treatment for early-stage oral cancer is lacking
Right now, there is no effective way to treat oral cancer early. Once detected, the options available are to “watch and wait” for progression or proceed straight to surgery. This can be complex and invasive due to the dense cluster of essential functions in the mouth, such as talking, breathing and eating.
Further treatments, including radiotherapy, chemotherapy or immunotherapy, are similarly late-stage, resource-heavy and poorly suited to early intervention.
Traditional photodynamic therapy (PDT) is an interesting non-invasive approach used in some cancers such as bladder and skin cancer, but it faces significant limitations. For example, patients must avoid light for days post-treatment due to photosensitivity. It is also complex and costly to implement. In particular, the use of PDT in oral cancer remains largely experimental and impractical for widespread use, putting it out of reach for many healthcare services.
There is also a logistical barrier. Oral cancers are often first spotted by dentists, not doctors. So, when a patient is referred into the healthcare system, they can fall through the cracks. There’s no continuous care pathway, and that (again) weakens the potential for early intervention.
The case for light-based prevention for oral cancers
There is a desperate need for a new generation of therapies that can aid the shift from treatment to prevention in oral cancer. These therapies must be accessible, simple to deploy and tailored to where and how mouth cancer occurs.
A new generation of light-based therapy overcomes the limitations of conventional PDT for treating oral cancer at the very earliest stages.
For example, using blue light – similar to that used in dentistry – offers key advantages over traditional red light. Blue light penetrates only shallow layers of mucosal tissues, enabling localized treatment with minimal systemic exposure. When paired with light-sensitive cytotoxic drugs delivered via topical gels, this method enables precise control over treatment – killing cancerous cells while sparing healthy tissue.
This approach offers the potential for faster recovery times and minimizes the need for complex infrastructure. Crucially, such tools could be administered in non-hospital settings with minimal training, increasing accessibility and reducing costs of treatment further.
Since most cases of mouth cancer begin as pre-cancerous lesions identified during routine dental examinations, there’s clear opportunity to develop tools that can be used in the dentist’s chair – stopping oral cancer before it takes hold.
With appropriate deployment, there is a real opportunity for tools like this to become as essential to oral cancer prevention as Human Papillomavirus screening and vaccination have been for cervical cancer.
Integrating oral cancer into the prevention revolution
If we believe in early detection and prevention for cancers like cervical and colorectal, then oral cancer cannot be left behind. Innovation should not serve only advanced treatments for wealthier settings, but enable early, accessible solutions where the burden is greatest.
It’s time to reframe how we think about mouth cancer. This is not a rare, late-stage problem. We already have the tools and scientific knowledge to act earlier, and we know that early action saves lives. The shift to early detection and prevention is transforming outcomes in other areas of cancer care – oral cancer must be part of that shift too.