High-Throughput Retinal Organoids: A New Vision for Therapy Development
The retina is one of the most intricate tissues in the body, comprising over 100 cell types.
A miniature retina with major impact
Imagine cultivating thousands of tiny, self-organizing eyes in a dish—retinal organoids that mirror the complexity of human vision. That’s the reality in Dr. Magdalena Renner’s lab, where cutting-edge stem cell technology and tissue engineering are converging to unlock new treatments for blinding diseases.
Speaking at Technology Networks’ recent “Innovations in Disease Modeling 2025” symposium, Renner, a leading expert in 3D organoid systems, detailed how her team has overcome longstanding barriers in retinal organoid production, enabling large-scale drug testing and long-term disease modeling.
Building the retina from scratch
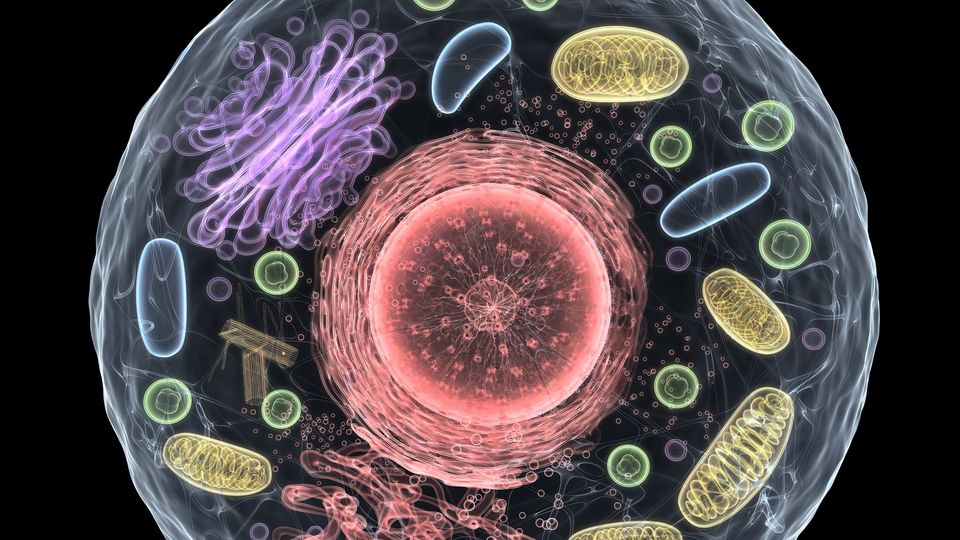
The retina is one of the most intricate tissues in the body, comprising over 100 cell types arranged in multilayered networks. In diseases such as retinitis pigmentosa, age-related macular degeneration (AMD) and glaucoma, specific retinal cells degenerate, often leading to permanent vision loss.
To model these conditions, Renner’s lab uses human induced pluripotent stem cells (iPSCs) to generate retinal organoids – tiny, spherical tissues that mimic the architecture and function of the human retina. These organoids contain all major retinal cell types, including rod and cone photoreceptors, bipolar cells, Müller glia and retinal pigment epithelial (RPE) cells.
Using single-cell RNA sequencing, Renner’s team validated that “organoid cell types are transcriptomically similar to cells of the adult human retina,” and, crucially, disease genes are expressed in the same cell types. This makes retinal organoids an ideal platform for disease modeling and therapeutic screening.
From three to thousands: Scaling up organoid production
While the scientific community has long recognized the potential of organoids, producing them in large numbers with consistent quality has remained a challenge, until now.
Initially, Renner could generate just three retinal organoids per well. However, by introducing two key innovations – controlled embryoid body (EB) formation and “checkerboard scraping” – her lab now achieves thousands per well.
The EB step proved pivotal. “Embryoid body size was really important for the outcome of our retinal organoid differentiation protocols,” she noted. Some iPSC lines were highly sensitive to initial size, impacting organoid yield and quality.
By seeding single cells into agarose microwell arrays, the team standardized EB formation, vastly improving reproducibility.
Scraping also replaced time-consuming manual microdissection. “I was dissecting organoids for days for our single-cell RNA sequencing […] then most turned out to not develop really well,” Renner recalled. With checkerboard scraping, she now harvests hundreds of healthy organoids in a fraction of the time.
Screening for sight-saving compounds
With high-throughput production in place, Renner’s lab turned to screening. Partnering with Novartis’ FAST lab, they tested a 2,700-compound library for agents that protect cone photoreceptors – the cells responsible for daylight and color vision.
Cone degeneration was induced by depriving organoids of glucose, simulating metabolic stress. The team used viral vectors to express green protein fluorescence under a cone-specific promoter, enabling live imaging over time.
“In low glucose medium […] cone photoreceptors are dying,” Renner reported, with roughly 40% lost in one week.
Some compounds slowed cone death, while others accelerated it. Two candidates, dubbed “cone-saving kinase inhibitors 1 and 2,” significantly increased cone survival at both 7 and 14 days. Follow-up kinase profiling suggested their likely targets were casein kinase 1 and MAP kinase 11, respectively – opening the door for targeted neuroprotective therapies.
The HistoBrick revolution
To understand organoids in more detail, histology is essential, but traditional sectioning is slow, error-prone and wasteful.
Enter the “HistoBrick,” a 3D-printed embedding mold developed in collaboration with the Swiss Center for Electronics and Microtechnology (CSEM).
“We developed the HistoBrick for cryosectioning to increase the throughput of organoid histology,” Renner explained.
This innovation of Renner’s team allows for the parallel sectioning of up to 16 organoids in a single block, drastically reducing cost and effort. Importantly, organoid identity is preserved by location, enabling multiplexed analysis.
Standard embedding materials like OCT damaged delicate outer segments of
photoreceptors. The team found a better solution: a UV-curable mix of gelatin and PEG-DA that preserves morphology and enables precision sectioning.
“With the HistoBrick, we could analyze organoids cultured for almost two years,” Renner shared. Remarkably, they still displayed layered structures and viable photoreceptors at 98 weeks.
Toward aging models and beyond
One unexpected discovery was the presence of displaced cone photoreceptors in older organoids – a feature reminiscent of changes seen in aging human retinas. “Potentially, retinal organoids could be used also as a model that recapitulates some aspects of the aging retina,” Renner suggested.
This positions retinal organoids not only as tools for treating inherited retinal diseases but also for studying age-related degeneration and testing long-term drug effects.
The road ahead
Despite remarkable progress, challenges remain. Organoids lack vascularization and retinal ganglion cells deteriorate early, limiting their use in modeling some diseases. Enhancing organoid structure and functionality – perhaps through co-culture systems or improved differentiation protocols – is a key next step.
Renner is also working on automating organoid selection and culture, to address labor-intensive steps and variation.
“Someone has to come. So it would help to put organoids on some automated culture platforms,” she noted, highlighting the need for continuous innovation.
Her advice to the field? “Each project needs kind of its own organoids, depending on the question.”
Whether it’s screening, transplantation or modeling aging, retinal organoids are proving to be flexible, scalable and surprisingly resilient.
This content includes text that has been generated with the assistance of AI. Technology Networks’ AI policy can be found here.




